1. Title Page
1.1 Intro - Page 1

2. Course Menu
2.1 Main Menu

3. Introduction
3.1 Untitled Slide

Notes:
Medicare
Fraud & Abuse: Prevent, Detect, Report - Introduction
3.2 Intro – Page 1

Notes:
The Medicare Fraud
& Abuse: Prevent, Detect, Report course is brought to you by the Medicare
Learning Network®
3.3 Intro - Page 2

Notes:
The Medicare Learning Network®
(MLN) offers free educational materials for health care professionals on
Centers for Medicare & Medicaid Services (CMS) programs, policies, and
initiatives. Get quick access to the information you need.
· MLN Publications & Multimedia
· MLN Events & Training
· MLN News & Updates
3.4 Intro - Page 3

Notes:
Navigating and Completing This
Course
This WBT has course content,
reference documents, review questions, and an assessment. Successfully
completing this course requires an assessment score of 70% or higher.
This course uses cues at various
times to give additional information. The cues are hyperlinks, buttons,
rollovers, and pop-up windows. For more information on these cues, select Help
in the top left corner. The Reference button includes
resource documents and a glossary of defined terms within it. You may print
these materials at any time.
After successfully completing the
course, you’ll get instructions on how to get
your certificate.
Visit the Reference
page for disclaimers, a list of helpful websites, and frequently asked
questions (FAQs). You may find this information useful as you go through this
course.
Watch the embedded videos or read
the transcripts. Information in the videos helps you meet course learning
objectives.
3.5 Intro - Page 4

Notes:
Welcome to the Medicare Fraud &
Abuse: Prevent, Detect, Report Course!
This course educates health care
professionals about how to prevent, detect, and report Medicare fraud &
abuse.
Although there is no precise measure
of health care fraud, those who exploit Federal health care programs can cost
taxpayers billions of dollars while putting beneficiaries’ health and
welfare at risk. The impact of these losses and risks magnifies as Medicare
continues to serve a growing number of beneficiaries.
The Federal government aggressively
cracks down on fraud & abuse, but it needs your help. All health care
professionals must do their part to prevent fraud & abuse.
Please note: The information in this
course focuses on the Medicare FFS Program (also known as Original Medicare).
Many of the laws discussed apply to all Federal health care programs (including
Medicaid and Medicare Parts C and D). See Job Aid C for information on
fraud & abuse in Medicaid and Medicare Parts C and D.
3.6 Intro - Page 5

Notes:
Do Your Part, Get Informed!
Committing Fraud Is Not Worth It
· Medicare Trust Fund
recovered approximately $1.2 billion
· $232 million
recovered in Medicaid Federal money transferred to the Treasury
· The Federal
government convicted 497 defendants of health care fraud
· Department of
Justice (DOJ) opened 1,139 new criminal health care fraud investigations
· DOJ opened 918 new
civil health care fraud investigations
Consequences
· HHS OIG Criminal
Actions:
· FY 2016: 765
· FY: 2017: 766
· FY: 2018: 679
· HHS OIG Civil
Actions:
· FY 2016: 690
· FY 2017: 818
· FY 2018: 795
· 2,712 Exclusions
NOTE: All statistics cover FY 2018
unless otherwise noted.
3.7 Intro - Page 6

Notes:
Course Objectives
After completing this course, you
should correctly:
· Identify what
Medicare considers fraud & abuse
· Identify Medicare
fraud & abuse provisions and penalties
· Recognize Medicare
fraud & abuse prevention methods
· Recognize entities
that detect Medicare fraud & abuse
· Recognize how to
report Medicare fraud & abuse
3.8 Intro - Page 7

Notes:
Course Overview
This course consists of five
lessons:
· Lesson 1: Medicare
Fraud & Abuse explains fraud & abuse basics
· Lesson 2: Medicare
Fraud & Abuse Laws and Penalties outlines the laws and sanctions used to
fight fraud & abuse
· Lesson 3: Physician
Relationships with Payers, Other Providers, and Vendors describes methods to
prevent Medicare fraud & abuse
· Lesson 4: Medicare
Anti-Fraud and Abuse Partnerships and Agencies identifies the entities charged
with detecting Medicare fraud & abuse
· Lesson 5: Report
Suspected Medicare Fraud & Abuse describes how to report suspected Medicare
fraud & abuse, how to self-disclose violations, and the rewards available
for reporting fraud & abuse
Select the Continue Arrow to return
to the Course Menu. Then, select Lesson 1: Medicare Fraud & Abuse.
4. Lesson 1
4.1 Title Card

Notes:
Medicare Fraud & Abuse: Prevent,
Detect, Report
Lesson 1: Medicare Fraud & Abuse
4.2 Lesson 1: Medicare Fraud & Abuse

Notes:
Lesson 1: Medicare Fraud & Abuse
This lesson introduces the basic
Medicare fraud & abuse concepts and what you must know to detect it within
your organization. Fraud is a crime with serious consequences, including
exclusion from Federal health care programs, fines, and prison. It should take
about 10 minutes to complete this lesson.
In this lesson, you’ll
learn about:
· Medicare fraud
· Medicare abuse
This lesson includes Medicare fraud
& abuse examples.
In 2018, the Federal government won
or negotiated over $2.3 billion in health care fraud judgments and settlements.
4.3 Lesson 1: Learning Objectives

Notes:
Lesson 1: Learning Objectives
After completing this lesson, you
should correctly:
· Identify Medicare
fraud basics
· Identify Medicare
abuse basics
· Recognize Medicare
fraud & abuse instances
4.4 Medicare Fraud & Abuse: A Serious Problem Requiring Your Attention

Notes:
Medicare Fraud & Abuse: A Serious Problem Requiring Your
Attention
Health care fraud can cost taxpayers
billions of dollars. The dollars lost to Medicare fraud & abuse increase
the strain on the Medicare Trust Fund. The impact of these losses and risks
magnifies as Medicare continues to serve a growing number of people.
Schemes and fraudulent billing
practices not only cost taxpayers, they endanger the
health and welfare of beneficiaries. For example, dozens of patients got
medically unnecessary cardiac pacemakers implanted because of a
cardiologist-involved scam. The doctor convinced his patients to get the
pacemakers by telling them they would die, even though they had a non-fatal
diagnosis. Thanks to anti-fraud efforts and education, law enforcement caught
and prosecuted the doctor. He was sentenced to 42 months in prison and ordered
to pay over $300,000 in fines and restitution.
4.5 Medicare Fraud & Abuse: A Serious Problem Requiring Your Attention (cont.)

Notes:
Medicare Fraud & Abuse: A Serious Problem Requiring Your
Attention (cont.)
To combat fraud & abuse, you
must know how to protect your organization from potential abusive practices,
civil liability, and possible criminal activity. You play a vital role in
protecting the integrity of the Medicare Program.
4.6 What Is Medicare Fraud?

Notes:
What Is Medicare Fraud?
· Knowingly
submitting, or causing to be submitted, false claims, or making
misrepresentations of facts to obtain a Federal health care payment (in other
words, fraud includes obtaining something of value through misrepresentation or
concealment of material facts)
· Knowingly
soliciting, receiving, offering, and/or paying remuneration to induce or reward
referrals for items or services reimbursed by Federal health care programs
· Making prohibited
referrals for certain designated health services
4.7 Examples of Medicare Fraud

Notes:
Examples of Medicare Fraud
Examples of actions that may
constitute Medicare fraud include:
· Knowingly billing
services not given or supplies not provided, including billing Medicare
appointments patients fail to keep
· Knowingly altering
claim forms, medical records, or receipts to get a higher payment
· Paying for
referrals of Federal health care program beneficiaries
To learn about real cases of
Medicare fraud and its consequences, see the case studies in Job Aid A.
4.8 Fraud in Practice

Notes:
Fraud in Practice
Anyone can commit Medicare fraud,
including people you know. Move the slider below to explore examples of Fraud
cases.
Medicare fraud extends beyond
medical professionals. Corporations and organized crime networks commit
Medicare fraud, unlawfully getting millions of Medicare Program dollars.
A major pharmaceutical manufacturer
pled guilty to misbranding and paid $600 million to resolve criminal and civil
liability from promoting a certain drug. Part of the settlement resolved
allegations the company misled doctors about the drug’s safety and
success and instructed them to miscode claims to ensure Federal health care
payments. The company also allegedly paid doctors kickbacks.
In another case, the government
charged 73 defendants when investigators uncovered an organized crime
ring’s scheme that allegedly involved more than $163 million in
fraudulent billings and identity theft impacting thousands of beneficiaries and
doctors.
Fraud Example 1
A hospital paid $8 million to settle
allegations it knowingly kept patients hospitalized, beyond the time considered
medically necessary, to increase its Medicare payments and maintain its
classification as a long-term acute care facility.
Fraud Example 2
A Durable Medical Equipment (DME)
business owner served 70 months in prison and paid $1.9 million in restitution
after pleading guilty to conspiracy to commit health care fraud and aggravated
identity theft. The DME company owner created several
different companies and submitted more than 1,500 false and fraudulent claims
to Medicare for unnecessary medical equipment.
Fraud Example 3
An oncologist and his wife paid $3.1
million to resolve allegations they jointly defrauded Medicare and other
Federal health care programs by overbilling medications and services and
billing medications and services not provided.
Fraud Example 4
A court sentenced a home health
provider to 168 months in prison for his role as one of the owners of a home
health agency that submitted about $45 million in false claims to Medicare.
Almost all his insulin claims billed twice-daily injections to purportedly
homebound diabetic patients. The investigation revealed most patients were not
homebound or insulin-dependent diabetics.
4.9 What is Medicare Abuse?

Notes:
What is Medicare Abuse?
Abuse describes practices that,
either directly or indirectly, result in unnecessary costs to the Medicare
Program. Abuse includes any practice inconsistent with providing patients
medically necessary services, meeting professionally recognized standards, and
charging fair prices.
Both fraud & abuse can expose
providers to criminal, civil, and administrative liabilities.
4.10 Examples of Abuse

Notes:
Examples of Abuse
Examples of actions that may
constitute Medicare abuse include:
· Billing unnecessary
medical services
· Charging excessively
for services or supplies
· Misusing claim
codes, such as upcoding or unbundling codes
To learn about real Medicare abuse
cases and its consequences, see the case studies in Job Aid B.
4.11 Program Integrity

Notes:
Program Integrity
Program Integrity includes a range
of activities to target the various causes of improper payments beyond fraud
& abuse. Select the vulnerability on the left to see the severity of the
consequences.
· Mistakes result in errors:
such as incorrect coding
· Inefficiencies result in waste:
such as ordering excessive diagnostic tests
· Bending the rules results in abuse:
such as improper billing practices (like upcoding)
· Intentional
deceptions
result in fraud, such as billing for services or supplies that were not provided
NOTE: The types of improper payments
are examples for educational purposes. Providers who engage in these practices
may be subject to administrative, civil, or criminal liability.
4.12 Lesson 1: Summary

Notes:
Lesson 1: Summary
· Fraud & abuse
drain billions of dollars from the Medicare Program each year and put
beneficiaries’ health and welfare at risk by exposing them to unnecessary
services, taking money away from care, and increasing costs.
· Fraud & abuse
jeopardize quality health care and services and threaten the integrity of the
Medicare Program by fostering the misconception that Medicare means easy money.
· Fraud & abuse
cost you as a health care provider and taxpayer. Fraud & abuse result in
waste and unintentionally financing criminal activities.
· Fraud includes, but
is not limited to, knowingly submitting false statements or making
misrepresentations of material facts to get a Federal
health care payment for which no entitlement would otherwise exist.
· Abuse describes
practices that, either directly or indirectly, result in unnecessary Medicare
Program costs.
4.13 Lesson 1 Review Title Card

Notes:
Review Questions
Lesson 1: Medicare Fraud & Abuse
After selecting an answer for a
question, select Submit Answer for feedback on the correct answer.
4.14 Review Question 1

Notes:
Review Question 1
Select the correct answer.
If you knowingly submit a false
statement of material fact to get a Medicare payment when no entitlement would
otherwise exist for someone other than yourself, you did not commit Medicare fraud.
· True
· False
4.15 Review Question 2

Notes:
Review Question 2
Select the correct answer.
Medicare abuse describes practices
that directly or indirectly result in unnecessary Medicare Program costs.
· True
· False
4.16 Review Question 3
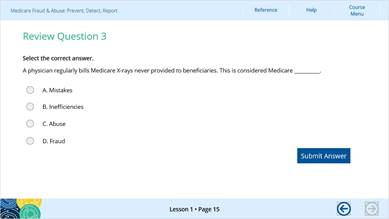
Notes:
Review Question 3
Select the correct answer.
A physician regularly bills Medicare
X-rays never provided to beneficiaries. This is considered Medicare __________.
· Mistakes
· Inefficiencies
· Abuse
· Fraud
4.17 You’ve completed Lesson 1: Medicare Fraud & Abuse

Notes:
You’ve completed Lesson
1: Medicare Fraud & Abuse
Now that you’ve
learned about Medicare fraud & abuse, let’s look at relevant Medicare
fraud & abuse laws. Lesson 2 explains provisions and penalties used to
fight and punish fraud & abuse and preserve Medicare Program integrity.
Select the Continue Arrow to return
to the Course Menu. Then, select Lesson 2: Medicare Fraud & Abuse Laws and
Penalties.
5. Lesson 2
5.1 Untitled Slide

Notes:
Medicare Fraud & Abuse: Prevent,
Detect, Report
Lesson 2: Medicare Fraud & Abuse
Laws and Penalties
5.2 Lesson 2: Medicare Fraud & Abuse Laws and Penalties

Notes:
Lesson 2: Medicare Fraud & Abuse
Laws and Penalties
In this lesson, you’ll
learn about laws the Centers for Medicare & Medicaid Services (CMS) and its
partners use to address fraud & abuse. Knowledge of fraud & abuse laws
helps you partner in preventing these activities, which drains billions of
dollars from the Medicare Program, endangers its integrity, drives up health
care costs, and compromises beneficiary health care services. This lesson should
take you about 35 minutes to complete.
In this lesson, you’ll
learn about:
· Federal laws
governing fraud & abuse
· Penalties for fraud
& abuse
5.3 Lesson 2: Learning Objectives

Notes:
Lesson 2: Learning Objectives
After completing this lesson, you
should correctly
· Identify these
fraud & abuse Federal laws:
· Federal Civil False
Claims Act (FCA)
· Anti-Kickback
Statute (AKS)
· Physician
Self-Referral Law (Stark Law)
· Criminal Health
Care Fraud Statute
· Exclusion Statute
· Civil Monetary
Penalties Law (CMPL)
· Recognize civil and
criminal fraud penalties
Use
Job Aid F as a resource for the laws discussed in
this lesson.
5.4 Medicare Fraud & Abuse Laws

Notes:
Medicare Fraud & Abuse Laws
The FCA, AKS, Physician
Self-Referral Law (Stark Law), Criminal Health Care Fraud Statue, Social
Security Act, which includes the Exclusion Statute, and CMPL, are the main laws
that address Medicare fraud & abuse and specify the criminal, civil, and
administrative penalties the government imposes on those committing fraud &
abuse. Violations may result in:
· Medicare-paid
claims recoupment
· Civil Monetary
Penalties (CMPs)
· Exclusion from
Federal health care programs participation
· Criminal and civil
liability
These
laws prohibit Medicare Part C and Part D and Medicaid fraud & abuse.
Let’s take a closer look at Medicare fraud &
abuse laws.
5.5 False Claims Act

Notes:
False Claims Act
The FCA (31 United States Code [U.S.C.] Sections 3729-3733) protects the
Federal government from being overcharged or sold substandard goods or
services. The FCA imposes civil liability on any person who knowingly submits,
or causes the submission of, a false or fraudulent claim to the Federal
government. The terms “knowing” and “knowingly” mean a
person has actual knowledge of the information or acts in deliberate ignorance
or reckless disregard of the truth or falsity of the information related to the
claim.
There is also a criminal FCA (18 U.S.C. Section 287). Criminal penalties for submitting false
claims may include prison, fines, or both.
Example: A physician
knowingly submits claims to Medicare for medical services not provided or for a
higher level of medical services than provided.
5.6 Anti-Kickback Statute

Notes:
Anti-Kickback Statute
The AKS (42 U.S.C. Section 1320a-7b(b)) makes it a crime to knowingly and
willfully offer, pay, solicit, or receive any remuneration directly or
indirectly to induce or reward referrals of items or services reimbursable by a
Federal health care program. Remuneration includes anything of value such as
cash, free rent, expensive hotel stays and meals, and excessive compensation
for medical directorships or consultations.
Criminal penalties and
administrative sanctions for violating the AKS may include fines, imprisonment,
and exclusion from participating in Federal health care programs.
The Code of Federal Regulations
(CFR) at 42 CFR Section 1001.952 sets the safe
harbor regulations and describes various payments and business practices that
may satisfy regulatory requirements and may not violate AKS. Go to the Safe Harbor Regulations webpage for more information.
Example: A provider gets
cash or below-fair-market-value rent for medical office space in exchange for
referrals.
5.7 Physician Self-Referral Law (Stark Law)

Notes:
Physician Self-Referral Law (Stark
Law)
The Physician Self-Referral Law
(Stark Law (42 U.S.C. Section 1395nn) prohibits a
physician from referring certain “designated health services” (for
example, clinical laboratory services, physical therapy, and home health services),
payable by Medicare or Medicaid, to an entity where the physician (or an
immediate family member) has an ownership/investment interest or has a
compensation arrangement, unless an exception applies.
Penalties for physicians who violate
the Stark Law include fines, repayment of claims, and potential exclusion from
participation in Federal health care programs.
Review the Code List for Certain Designated Health Services (DHS) webpage and
request an advisory opinion if you have questions on specific
scenarios.
Review the Comparison of the Anti-Kickback Statute and Stark Law for a simplified
overview of the two laws.
Example: A provider refers
a patient for a designated health service to a clinic where the physician (or
an immediate family member) has an investment interest.
5.8 Criminal Health Care Fraud Statute

Notes:
Criminal Health Care Fraud Statute
The Criminal Health Care Fraud
Statute (18 U.S.C. Section 1347) prohibits
knowingly and willfully executing, or attempting to execute, a scheme or lie
about the delivery of, or payment for, health care benefits, items, or services
to either:
· Defraud any health
care benefit program
· Get (by means of
false or fraudulent pretenses, representations, or promises) the money or
property owned by, or under the custody or control of, a health care benefit program
Penalties for violating the Criminal
Health Care Fraud Statute may include fines, prison, or both.
Now, let’s
review Medicare fraud & abuse penalties for violating the FCA, AKS, Stark
Law, or the Criminal Fraud Statute.
Example: Several doctors
and medical clinics conspired to defraud the Medicare Program by submitting
claims for medically unnecessary power wheelchairs.
5.9 Medicare Fraud & Abuse Penalties

Notes:
Medicare Fraud & Abuse Penalties
Beyond paying restitution to CMS for
money acquired fraudulently, Medicare fraud & abuse penalties may include
exclusions, CMPs, and sometimes criminal sanctions-including fines and
prison-against health care providers and suppliers who violate the FCA, AKS, Physician
Self-Referral Law (Stark Law), or Criminal Health Care Fraud Statute.
Now, let’s
look at Medicare Program exclusions and how they affect providers.
5.10 Exclusion Statute

Notes:
Exclusion Statute
The Exclusion Statute (42 U.S.C. Section 1320a-7) requires the U.S. Department of Health
& Human Services (HHS) Office of Inspector General (OIG) to exclude health
care providers and suppliers convicted of certain offenses from participating
in Federal health care programs. OIG may also impose permissive exclusions on
several other grounds.
Visit the OIG Exclusions Program webpage for more information.
5.11 Exclusion Statute: Referrals

Notes:
Exclusion Statute: Referrals
Excluded providers may not
participate in Federal health care programs for a designated period but may
refer a patient to a non-excluded provider if the excluded provider does not
furnish, order, or prescribe services for the referred patient. In this case,
the non-excluded provider must treat the patient and independently bill Federal
health care programs for items or services provided. Covered items or services
from a non-excluded provider to a Federal health care
program beneficiary are payable, even when an excluded provider referred the
patient.
5.12 Mandatory Exclusion

Notes:
Mandatory Exclusion
For certain offenses, the OIG must
impose an exclusion. Mandatory exclusions stay in effect for a minimum of 5
years; however, aggravating factors may lead to an even longer or permanent
exclusion. Providers and suppliers face mandatory exclusions if convicted of
these offenses:
Mandatory Exclusion Offense
· Medicare or Medicaid
fraud and criminal offenses related to the delivery of items or services under
a Federal or State health care program
· Criminal offenses
related to patient abuse or neglect
· Felony convictions
for other health care-related fraud, theft, embezzlement, breach of fiduciary
responsibility, or other financial misconduct connected to the delivery of a
health care item or service
· Felony convictions
for unlawful manufacture, distribution, prescription, or dispensing controlled substances
5.13 Permissive Exclusion

Notes:
Permissive Exclusion
The OIG may impose exclusions for
offenses not under a mandatory exclusion. Permissive exclusions vary in length.
The OIG may issue permissive
exclusions for various actions.
For a complete list of permissive
exclusions, review 42 U.S.C. Section 1320a-7.
Permissive Exclusion Examples
· Misdemeanor health
care fraud convictions other than Medicare or Medicaid fraud
· Misdemeanor
convictions for unlawfully manufacturing, distributing, prescribing, or
dispensing controlled substances
· Revocation,
suspension, or health care license surrender for reasons of professional
competence, professional performance, or financial integrity
· Providing unnecessary
or substandard service
· Convictions for
obstructing an investigation or audit
· Engaging in
unlawful kickback arrangements
· Defaulting on
health education loan or scholarship obligations
5.14 OIG List of Excluded Individuals/Entities

Notes:
OIG List of Excluded
Individuals/Entities
The OIG List of Excluded
Individuals/Entities (LEIE) publicly lists individuals and entities currently
excluded from participation in all Federal health care programs. Providers and
contracting entities must check the program exclusion status of individuals and
entities in the LEIE before entering employment or contractual relationships.
Health care providers that knowingly
hire an excluded party are subject to potential FCA liability and CMPs.
Medicare will not pay for services by an excluded party, with certain exceptions.
Prior to hiring an individual, purchasing supplies, or contracting with an
entity (and periodically thereafter), health care providers should use the OIG
LEIE to check program exclusion status.
5.15 Search the List of Excluded Individuals/Entities

Notes:
Search the List of Excluded
Individuals/Entities
The LEIE is accessible through a
searchable online database. It identifies parties excluded from Medicare
reimbursement. The list includes information about the provider’s
specialty, exclusion type, and
exclusion date.
Access the LEIE
on the OIG website.
5.16 General Services Administration’s System for Award Management

Notes:
General Services
Administration’s System for Award Management
The General Services Administration
(GSA) consolidated several Federal procurement systems into one new system-the System for Award Management (SAM). SAM incorporated the Excluded Parties
List System (EPLS) and includes information on entities:
· Debarred or
proposed for debarment
· Disqualified from
certain types of Federal financial and non-financial assistance and benefits
· Disqualified from
getting Federal contracts or certain subcontracts
· Excluded
· Suspended
OIG compliance guidance encourages
health care providers to check the SAM prior to hiring an individual,
purchasing durable medical equipment (DME), supplies, or contracting with an
entity (and periodically thereafter). Read the GSA fact sheet How do I search for an exclusion? for detailed instructions.
Remember, health care providers
should check the LEIE and the SAM before making employment and contract
decisions. You cannot get Federal payment or compensation for services provided
by individuals and organizations listed on the LEIE and the SAM.
Now, let’s
look closer at the exclusion payment denial.
5.17 Exclusion: Denial of Payment

Notes:
Exclusion: Denial of Payment
An OIG exclusion means Federal
health care programs do not pay for items or services given, ordered, or
prescribed by an excluded individual or entity. Federal health care programs
also make no payment to the excluded individual, anyone who employs or contracts
with the excluded individual, and a hospital or other provider where the
excluded individual provides services.
The exclusion applies regardless of
who submits the claims for payment and applies to all administrative and
management services given by the excluded individual.
For example, Federal health care
programs do not make payment if:
· A hospital employs
an excluded nurse who provides items or services to Federal health care program
beneficiaries, even
if the nurse’s services are not separately billed and are paid as part of
a Medicare diagnosis-related group payment the hospital gets
· The excluded nurse
violates their exclusion thereby causing the hospital to submit claims for
items or services they provide
During an exclusion period, the excluded
individual or entity may face additional penalties for submitting or causing
the submission of claims to a Federal health care program. The excluded individual
or entity is susceptible to CMP liability as well as reinstatement denial to
the Federal health care programs, including Medicare. Exceptions to payment
denial apply in specific situations.
5.18 Exclusion: Denial of Payment Exceptions

Notes:
Exclusion: Denial of Payment
Exceptions
If a beneficiary submits claims for
items or services given, ordered, or prescribed by an excluded individual or
entity in any capacity after the effective date of the exclusion:
· Medicare pays the
first claim submitted by the beneficiary and immediately gives the beneficiary
notice of the exclusion
· Medicare makes no
payment for the beneficiary items or services given more than 15 days after the
date of the notice or after the effective date of the exclusion, whichever is later
The same process applies when labs
or DME suppliers submit item or service claims ordered or prescribed by an
excluded individual or entity.
There are also exceptions for
certain inpatient hospital, skilled nursing facility, home health, and emergency
services detailed in the Medicare Program Integrity
Manual, Chapter 4,
Section 4.19.2.6.
5.19 Exclusion: Reinstatement

Notes:
Exclusion: Reinstatement
Reinstating excluded entities and
individuals is not automatic once the specified exclusion period ends. Those
who want to participate in all Federal health care programs must apply for
reinstatement and get authorized notice from the OIG they granted reinstatement.
If the OIG denies reinstatement, the excluded party is eligible to re-apply
after 1 year.
Now, let’s
look at CMPs.
5.20 Civil Monetary Penalties

Notes:
Civil Monetary Penalties
CMPs apply to a variety of health
care fraud violations, and assessment of the CMP depends on the type of
violation. The CMP authorizes penalties up to $100,000 (in 2018) per violation,
and assessments of up to 3 times the amount claimed for each item or service,
or up to 3 times the amount of remuneration offered, paid, solicited, or
received. Violations that justify CMPs include:
· Presenting a claim
you know, or should know, is for an item or service not provided as claimed or
is false and fraudulent
· Violating the AKS
· Making false
statements or misrepresentations on applications or contracts to participate in
the Federal health care programs
CMP Inflation Adjustment
Each year, the Federal government
adjusts all CMPs for inflation. The adjusted amounts apply to civil penalties
assessed after August 1, 2016, and violations after November 2, 2015. Refer to 45 CFR 102.3
for the yearly inflation adjustments.
Now, let’s
look at civil prosecutions and penalties.
5.21 Civil Prosecutions and Penalties

Notes:
Civil Prosecutions and Penalties
Depending on the severity of the
violation, a civil suit or settlement may include any combination of the
following:
· A CMP for each item
or service in non-compliance (or higher amounts where applicable by statute)
· Payment up to 3
times the amount claimed for each item or service instead of damages sustained
by the Federal government
· Exclusion from all
Federal health care programs for a specified period
· An OIG Corporate
Integrity Agreement (CIA), which requires an individual or entity to carry out
a compliance program (including, for example, hiring a compliance officer,
developing written standards and policies, carrying out an employee training
program, and conducting annual audits and reviews)
In addition to civil prosecutions
and penalties, law enforcement may prosecute health care fraud and pursue
criminal convictions. Under the Affordable Care Act, the U.S. Sentencing
Commission may add offense levels for health care fraud crimes with more than
$1 million in losses. It is also a crime to obstruct fraud investigations.
Stay updated on the latest
enforcement actions on the OIG Criminal and Civil
Enforcement
webpage.
5.22 Lesson 2: Summary

Notes:
Lesson 2: Summary
· The FCA, AKS,
Physician Self-Referral Law (Stark Law), Criminal Health Care Fraud Statute,
the Social Security Act which includes, the Exclusion Statute, and the CMPLs,
are the main Federal laws that address Medicare fraud & abuse.
· FCA: The FCA
imposes civil liability on a person who knowingly submits, or causes the
submission of, a false or fraudulent claim to the Federal government. The
“knowing” standard includes acting in deliberate ignorance or
reckless disregard of the truth related to the claim.
· Anti-Kickback
Statute: The AKS prohibits knowingly and willfully offering, paying,
soliciting, or getting remuneration in exchange for Federal health care program
business referrals.
· Physician
Self-Referral Law (Stark Law): The Physician Self-Referral Law (Stark Law)
prohibits physicians from referring Medicare beneficiaries for designated
health services to an entity where the physician (or an immediate family
member) has an ownership/investment interest or a compensation arrangement, unless an exception applies.
· Criminal Health
Care Fraud Statute: The Criminal Health Care Fraud Statute prohibits knowingly
and willfully executing, or attempting to execute, a scheme or lie for
delivering, or paying for, health care benefits, items, or services to defraud
a health care benefit program, or to get (by means of false or fraudulent
pretenses, representations, or promises) the money or property owned by, or
under the custody or control of, a health care benefit program.
· Exclusion Statute:
The Exclusion Statute prohibits the excluded individual or entity from
participating in all Federal health care programs. The exclusion means no
Federal health care program pays for items or services given, ordered, or
prescribed by an excluded individual or entity.
· Civil Monetary
Penalties (CMPs): CMPs apply to a variety of conduct violations,
and assessing the CMP amount depends on the violation. Penalties up to
$100,000 (in 2018) per violation may apply. CMPs may also include an assessment
of up to 3 times the amount claimed for each item or service, or up to 3 times
the amount offered, paid, solicited, or got.
· Providers and
contracting entities must check for program exclusion status prior to entering
employment or contractual relationships using the OIG LEIE. OIG recommends
checking SAM as well.
· Civil and criminal
prosecutions can result in a variety of fines, exclusion, CIAs, and even prison
in criminal cases.
5.23 Lesson 2 Review Title Card

Notes:
Review Questions
Lesson 2: Medicare Fraud & Abuse
Laws and Penalties
After selecting an answer for a
question, select Submit Answer for feedback on the correct answer.
5.24 Review Question 1

Notes:
Review Question 1
Select the correct answer.
The Federal fraud & abuse laws
are the False Claims Act (FCA), the Anti-Kickback Statute, the Physician
Self-Referral Law (Stark Law), Criminal Health Care Fraud Statute, Social
Security Act, and the Civil Monetary Penalties Law (CMPL).
· True
· False
5.25 Review Question 2

Notes:
Review Question 2
Select the correct answer.
Which of the following is NOT a
possible penalty for Medicare fraud or abuse?
· A. Exclusion from
participating in all Federal health care programs
· B. Imprisonment in
criminal cases
· C. Civil Monetary
Penalties (CMPs) up to $500,000 per violation
5.26 Completed Lesson 2

Notes:
You’ve completed Lesson
2: Medicare Fraud & Abuse Laws and Penalties
Now that you’ve
learned about Medicare fraud & abuse basic laws and penalties, let’s
look at preventing Medicare fraud & abuse.
Select the Continue Arrow to return
to the Course Menu. Then, select Lesson 3: Physician Relationships with Payers,
Other Provider, and Vendors.
6. Lesson 3
6.1 Lesson 3 Title Card

Notes:
Medicare Fraud & Abuse: Prevent,
Detect, Report
Lesson 3: Physician Relationships
with Payers, Other Providers, and Vendors
6.2 Lesson 3: Introduction

Notes:
Lesson 3: Physician Relationships
with Payers, Other Providers, and Vendors
In this lesson, you’ll
learn how physician relationships with payers, other providers, and vendors can
prevent Medicare fraud & abuse. It should take about 15 minutes to
complete.
In this lesson, you’ll
learn about:
· How you can help
prevent Medicare fraud & abuse
· How compliance with
Medicare laws, regulations, and policies prevent fraud & abuse
· Continuing
education available on Medicare laws, regulations, and polices about fraud
& abuse prevention
6.3 Lesson 3: Learning Objectives

Notes:
Lesson 3: Learning Objectives
After completing this lesson, you
should correctly:
· Identify ways your
relationships with payers, other providers, and vendors prevent fraud & abuse
· Identify ways to
comply with Medicare laws, regulations, and policies to prevent fraud & abuse
· Identify continuing
education available on Medicare laws, regulations, and policies
6.4 Physician Relationships with Payers, Other Providers, and Vendors

Notes:
Physician Relationships with Payers,
Other Providers, and Vendors
The U.S. health care system relies
on third party payers to pay most medical bills on behalf of patients. These
payers understand Federal fraud & abuse laws apply when the government
covers items or services provided to Medicare and Medicaid beneficiaries. This
lesson focuses on:
· Physician
Relationships with Payers
· Physician
Relationships with Other Providers
· Physician
Relationships with Vendors
· Continuing Medical
Education on Medicare laws, regulations, and policies
6.5 You Can Help Prevent Medicare Fraud & Abuse

Notes:
You Can Help Prevent Medicare Fraud
& Abuse
As a health care provider, you play
a vital role in the fight against Medicare fraud & abuse. Help prevent
Medicare fraud &
abuse by:
· Checking the List
of Excluded Individuals/Entities (LEIE) and System for Award Management (SAM)
before making hiring and contracting decisions
· Providing only
medically necessary, high quality Medicare beneficiary services
· Accurately coding
and billing Medicare services
· Maintaining
accurate and complete Medicare beneficiary medical records
· Understanding and
complying with the Anti-Kickback Statute and Physician Self-Referral Law (Stark
Law) when making investments or doing business with vendors
·
6.6 You Can Help Prevent Medicare Fraud & Abuse (continued)

Notes:
You Can Help Prevent Medicare Fraud
& Abuse (continued)
Fraud & abuse also exist in
Medicare Part C, Part D, and Medicaid, especially involving “dual eligibles.”
For more information, see Job Aid
C and Job Aid D.
Now let’s
look at physicians’ relationships with payers related to accurate coding,
billing, documentation, investments, and physician recruitment.
6.7 Accurate Coding and Billing

Notes:
Accurate Coding and Billing
As a physician, payers trust you to
provide medically necessary, cost-effective, quality care. When you submit
claims for Medicare services, you certify you earned the payment and complied
with billing requirements. If you knew, or should have known, you submitted a
false claim, this is an illegal attempt to collect payment. Examples of
improper claims include:
Examples of improper claims include:
· Billing
codes that reflect a more severe illness than existed or a more expensive
treatment than provided
· Billing
medically unnecessary services
· Billing
services not provided
· Billing
services performed by an improperly supervised or unqualified employee
· Billing
services performed by an employee excluded from participation in Federal health
care programs
· Billing
services of such low quality they are virtually worthless
· Billing
separately for services already included in a global fee, like billing an
Evaluation and Management (E/M) service the day after surgery
6.8 Physician Documentation

Notes:
Physician Documentation
Maintain accurate and complete
records of the services you provide. Make sure your documentation supports your
claims for payment. Good documentation practices help ensure your patients get
appropriate care and allow other providers to rely on your records for
patients’ medical histories.
The Medicare Program may review
beneficiaries’ medical records. Good documentation helps address any
challenges raised about the integrity of your claims. You may have heard the
saying regarding malpractice litigation: “If you didn’t document
it, it’s the same as if you didn’t do it.” The same can be
said for Medicare billing.
6.9 Physician Documentation (continued)

Notes:
Physician Documentation (continued)
Medicare pays for many physician
services using E/M codes. These codes identify the level of service and
pay new patient codes at a higher level than established patients. Billing an
established patient follow-up visit using a higher-level E/M code is upcoding.
Another example of E/M upcoding is
misusing modifier -25, which allows additional payment for a significant,
separately identifiable E/M service provided on the same day of a procedure or
other service. Upcoding occurs when a provider uses modifier -25 to claim
payment for a medically unnecessary E/M service, an E/M service not distinctly
separate from the procedure provided, or an E/M service not above and beyond
the care usually associated with the procedure.
CPT only copyright 2018 American
Medical Association. All rights reserved.
6.10 Physician Investments in Health Care Business Ventures

Notes:
Physician Investments in Health Care
Business Ventures
Some physicians who invest in
business ventures with outside parties (for instance, imaging centers, laboratories,
equipment vendors, or physical therapy clinics) refer more patients for
services provided by those parties than physicians who do not invest. These
business relationships may improperly influence or distort physician
decision-making and result in improper patient-steering to a therapy or service
where a physician has a financial interest.
Excessive and medically unnecessary
referrals waste Federal government resources and can expose Medicare
beneficiaries to harmful, unnecessary services. Many of these investment
relationships have legal risks under the AKS and Stark Law.
If a health care business invites
you to invest and might be a place where you would refer your patient,
investigate the relationship thoroughly before proceeding.
6.11 Physician Recruitment

Notes:
Physician Recruitment
Hospitals and other health systems
may provide a physician-recruitment incentive to induce providers or practices
to join their medical staff. Often, such recruitment efforts fill a legitimate
“clinical gap” in a medically underserved area where attracting
physicians may be difficult without financial incentives.
Some hospitals, however, may offer
incentives which cross the line into an illegal arrangement with legal
consequences for the provider and the hospital.
A hospital may pay a provider a fair
market-value salary as an employee or pay them a fair market value for specific
services they provide to the hospital as an independent contractor. The
hospital may not offer money, free or below-market rent for a medical office, or engage in similar activities designed to
influence referral decisions.
Now let’s
look at physician relationships with vendors related to transparency and
conflict of interest.
6.12 Physician Relationships with Vendors

Notes:
Physician Relationships with Vendors
Many drug
and biologic companies provide free product samples to physicians. It is legal
to give these samples to patients free of charge, but it is illegal to sell the
samples. The Federal government prosecutes physicians for billing Medicare for
free samples. Implement reliable systems to safely store free samples and
ensure they remain separate from your commercial stock.
Some pharmaceutical and device
companies use sham consulting agreements and other arrangements to buy physician
loyalty. If you have opportunities to work as a consultant for the drug or
device industry, evaluate the link between the services you provide and the
compensation you get. Test the appropriateness of any proposed relationship by
asking yourself:
· Does the company
really need your specific expertise or input?
· Does the
company’s monetary compensation represent a fair, appropriate, and
commercially reasonable exchange for
your services?
· Is it possible the
company is paying for your loyalty, so you prescribe or use its products?
6.13 Federal Open Payments Program

Notes:
Federal Open Payments Program
The Federal Open Payments Program is
a national disclosure program that promotes health care transparency by making
financial relationships between health care providers and drug and medical
device companies available to the public. The Open Payments data includes
payments and other transfers of value such as gifts, honoraria, consulting
fees, research grants, travel reimbursements, and other payments drug or device
companies provide to physicians and teaching hospitals. The data also includes
ownership and investment interests held by physicians or their immediate family
members in reporting entities.
Data from a given year must be
reported by drug and device companies by March 31 of the following year. CMS
posts Open Payments data on or by June 30 each year. The public data is
accessible via the Open Payments Search Tool. CMS closely
monitors this process to ensure reported data integrity.
Visit Open Payments
for more information.
6.14 Conflict-of-Interest Disclosures

Notes:
Conflict-of-Interest Disclosures
Rules about disclosing and managing
conflicts of interest come from a variety of sources, including grant funders,
such as States, universities, and the National Institutes of Health (NIH), and
from the U.S. Food and Drug Administration (FDA) when you submit data to
support marketing approval for new drugs, devices, or biologics.
If you are uncertain whether a
conflict exists, ask yourself if you would want the arrangement to appear in
the news.
6.15 Education on Medicare Laws, Regulations, and Policies

Notes:
Education on Medicare Laws,
Regulations, and Policies
The Medicare Learning Network®
(MLN) offers a variety of health care training and educational materials
explaining Medicare policy. The MLN delivers planned and coordinated provider
education through various media, including MLN Matters® Articles, fact
sheets and booklets, web-based training courses, videos, and podcasts. Visit
the MLN for a list of educational products.
The MLN Provider Compliance webpage contains educational products
informing Medicare Fee-For-Service (FFS) Providers how to avoid common Medicare
Program billing errors and other improper activities.
The OIG Compliance
webpage provides education, compliance guidance, advisory opinions, and
training resources.
Medicare Administrative Contractor (MAC)
Provider Outreach and Education (POE) Programs offer providers and suppliers
education on the fundamentals of the Medicare Program.
6.16 Lesson 3: Summary

Notes:
Lesson 3: Summary
You play a vital role in detecting
fraud. Your actions can help protect the Medicare Trust Fund. Be sure to
review:
· Your relationships
with payers related to accurate coding, billing, and documentation
· Your relationships
with other providers related to investments and recruitment
· Your relationships
with vendors related to transparency and conflict of interest
· Training available
related to Medicare laws, regulations, and policies
6.17 Lesson 3 Review Title Card

6.18 Review Question 1

Notes:
Review Question 1
Select the correct answer.
You can help prevent Medicare fraud
& abuse by __________.
· A. Providing only
medically necessary, high quality services to Medicare beneficiaries
· B. Properly
documenting all services provided to Medicare beneficiaries
· C. Correctly
billing and coding services provided to Medicare beneficiaries
· D. All of the above
6.19 Review Question

Notes:
Review Question 2
Select the correct answer.
The Medicare Learning Network®
provides a variety of __________ for health care professionals.
· A. Coding Rules
· B. Training and
educational products
· C. Regulations
· D. Enrollment forms
6.20 You’ve completed Lesson 3: Physician Relationships with Payers, Other Providers, and Vendors

Notes:
You’ve completed Lesson
3: Physician Relationships with Payers, Other Providers, and Vendors
Now that you’ve
learned how your relationships with payers, other providers, and vendors
prevent fraud & abuse, let’s look at Medicare anti-fraud partnerships
and agencies.
Select Continue Arrow to return to
the Main Menu. Then, select Lesson 4: Medicare Anti-Fraud and Abuse
Partnerships
and Agencies.
7. Lesson 4
7.1 Lesson 4 Title Card

Notes:
Medicare Fraud & Abuse: Prevent,
Detect, Report
Lesson 4: Medicare Anti-Fraud and
Abuse Partnerships and Agencies
7.2 Lesson 4: Review

Notes:
Lesson 4: Medicare Anti-Fraud and
Abuse Partnerships and Agencies
In this lesson, you’ll
learn about the entities and methods used to detect fraud & abuse. It
should take about 15 minutes to complete this lesson.
In this lesson, you will learn
about:
· Efforts by the
Centers for Medicare & Medicaid Services (CMS) to detect fraud & abuse
in the Medicare program
· Data analysis, the
Fraud Prevention System (FPS), and the Integrated Data Repository (IDR)
· Entities that
conduct pre-payment and/or post-payment claims review to detect Medicare fraud
& abuse
· Entities that
investigate suspected Medicare fraud & abuse
The return on investment from
2016-2018 was $4.00 for every $1.00 dollar spent on fighting health care fraud
& abuse.
7.3 Lesson 4: Learning Objectives

Notes:
Lesson 4: Learning Objectives
After completing this lesson, you
should correctly:
· Recognize efforts
by CMS to detect fraud & abuse in the Medicare program
· Recognize entities
conducting pre-payment and/or post-payment claims review
· Recognize entities
investigating suspected Medicare fraud & abuse
7.4 Health Care Fraud Prevention Partnership

Notes:
Health Care Fraud Prevention
Partnership
The Health Care Fraud Prevention Partnership (HFPP) is a
voluntary, public-private partnership including 132 partners from the Federal
government, state agencies, law enforcement, private health insurance plans,
employer organizations, and health care anti-fraud associations. Their goal is
to identify and reduce fraud, waste, and abuse across the health care sector
through collaboration, data and information sharing, and cross-payer research
studies. The HFPP also performs sophisticated industry-wide analytics to detect
and predict fraud schemes.
7.5 The Centers for Medicare & Medicaid Services

Notes:
The Centers for Medicare &
Medicaid Services
CMS is the Federal
agency within the Department of Health and Human Services (HHS) that
administers the Medicare and Medicaid programs.
· Accreditation
Organizations
· Medicare
beneficiaries and caregivers
· Physicians,
suppliers, and other health care providers
· Office of
Inspector General (OIG)
· Federal
Bureau of Investigation (FBI)
· Contractors
Let’s review the
contractors that assist with CMS efforts to prevent and detect fraud.
7.6 Claim-Reviewing Entities

Notes:
Claim-Reviewing Entities
CMS authorizes several different
contractors to conduct pre-payment and/or post-payment reviews of claims. These
include:
· Comprehensive
Error Rate Testing (CERT) Contractors
· Medicare
Administrative Contractors (MACs)
· Recovery
Audit Contractors (RACs)
· Supplemental
Medical Review Contractor (SMRC)
· Unified
Program Integrity Contractors (UPICs)
If one of these entities contacts
you, respond within the specified timeframe and with all requested
documentation supporting the claim service(s) medical necessity. This ensures
accurate payment of the claim(s) under review and prevents payment recoupment
for claims correctly paid. Contact your MAC <http://go.cms.gov/MAC-website-list>
to find contact information for your review contractors.
7.7 Comprehensive Error Rate Testing Program

Notes:
Comprehensive Error Rate Testing
Program
The CERT Program
produces a national Medicare Fee-For-Service (FFS) error rate. CERT randomly
selects a statistically valid, random sample of Medicare FFS claims and reviews
those claims’ and related medical records’
compliance with Medicare coverage, payment, coding, and billing rules.
To accurately measure the
MACs’ performance and gain insight into error causes, CMS calculates a
national Medicare FFS paid claims error rate and an improper payment rate by
claim type and publishes the results of these reviews annually.
For example, here are the improper
payment rate and projected improper payment amounts by claim type for Fiscal
Year (FY) 2018. If you see your provider type on this list, refer to Job Aid D
for tips on avoiding fraud & abuse.
Service Type - Inpatient Hospitals,
Improper Payment Rate - 4.29%, Improper Payment Amount - $4.96B
Service Type - Durable Medical Equipment, Improper
Payment Rate - 35.54%, Improper Payment Amount - 2.59B
Service Type - Physician/Lab/Ambulance,
Improper Payment Rate - 10.68%, Improper Payment Amount - $10.47B
Service Type - Non-Inpatient
Hospital Facilities, Improper Payment Rate - 8.07%, Improper Payment
Amount - $13.60B
Service Type - Overall, Improper
Payment Rate - 8.12%, Improper Payment Amount - $31.62B
7.8 CERT Program FFS Improper Payment Rate

Notes:
CERT Program FFS Improper Payment Rate
The Medicare FFS Improper Payment
Rate is a good indicator of how Medicare FFS claims errors impact the Medicare
Trust Fund. CMS and MACs educate providers and suppliers on CERT-identified
high-risk areas.
For more information, visit the CERT Documentation Contractor website. The CERT Outreach and Education Task Force provides consistent, accurate
provider outreach and education to help reduce the improper payment rate.
7.9 Medicare Administrative Contractors

Notes:
Medicare Administrative Contractors
CMS, MACs, and other claim review
contractors identify suspected billing problems through error rates produced by
the CERT Program, vulnerabilities identified through the Recovery Audit
Program, analysis of claims data, and evaluation of other information (for
example, complaints).
CMS, MACs, and other claim review
contractors target Medical Review (MR) activities on problem areas based on the
severity of the problem. The SMRC conducts nationwide MR as directed by CMS.
This includes identifying underpayments and overpayments.
MR may occur before or after the MAC
makes a payment on the claim. MACs may review one or multiple claims at the
same time.
Some providers may go through probed
reviews or placed on Progressive Corrective Action (PCA) plans depending on the
extent of their billing errors.
7.10 Medicare FFS Recovery Audit Program

Notes:
Medicare FFS Recovery Audit Program
Medicare FFS Recovery Audit
Contractors (RACs) conduct post-payment claim reviews to detect improper
underpayments and overpayments. RACs may target claim reviews by service. Each
RAC website publishes its targeted services. Visit the Recovery Audit Program webpage for more information, including
Medicare Parts A and B Recovery Auditors contact information.
Also review the Quarterly Provider Compliance Newsletter for common
Medicare FFS Recovery Audit and CERT findings and tips for avoiding issues.
7.11 Parts C and D Recovery Audit Program

Notes:
Parts C and D Recovery Audit Program
CMS created the Parts C and D
Recovery Audit Program to identify and correct past improper payments to
Medicare providers. CMS also implemented procedures to help MACs prevent future
improper payments. Communication about audit results and trends leads to continuous
process improvement, more accurate payments, and helps plan sponsors correct
issues in a timely manner.
CMS designated one Recovery Auditor
to review payments for Medicare Part D. CMS will start the Recovery Audit
Program for Medicare Part C payments in the future. Visit the Parts C and D Recovery Audit Program webpage for more information.
Now that you’ve
learned about the entities that review claims, let’s discuss entities
that provide analytical support to CMS to detect fraud & abuse activities.
7.12 Analytical Entities

Notes:
Analytical Entities
Within CMS, the Center for Program Integrity (CPI) promotes Medicare integrity through
audits, policy reviews, and identifying and monitoring program vulnerabilities.
CPI oversees CMS’ collaboration with key stakeholders on detecting,
deterring, monitoring, and combating fraud & abuse issues.
In 2010, HHS and CMS launched the
Fraud Prevention System (FPS), a state of-the-art predictive analytics
technology that runs Medicare FFS claims predictive algorithms and other
analytics prior to payment to detect potentially suspicious claims and patterns
that may constitute fraud & abuse.
7.13 Fraud Prevention System

Notes:
Fraud Prevention System
The FPS uses sophisticated analytics
to prevent and detect fraud & abuse in the Medicare FFS Program. It provides
a comprehensive view of Medicare FFS provider and beneficiary activities to
identify and analyze provider networks, billing patterns, beneficiary usage
patterns, and patterns representing a high risk of fraudulent activity.
The FPS is fully integrated with the
Medicare FFS claims processing system and uses other data sources, such as the
Integrated Data Repository (IDR).
· A home health
agency in Florida billed services never provided. Due to the FPS, CMS placed
the home health agency on pre-payment review and payment suspension, referred
the agency to law enforcement, and ultimately revoked the agency’s Medicare
enrollment.
· In Texas, the FPS
identified an ambulance company submitting claims for non-covered services and
services not given. Medicare revoked the ambulance company’s enrollment.
· The FPS identified
an Arizona medical clinic with questionable billing practices, such as billing
excessive units of service per beneficiary per visit. The physicians delivered
repeated and unnecessary neuropathy treatments to beneficiaries. CMS revoked
the medical clinic’s Medicare enrollment.
7.14 Integrated Data Repository

Notes:
Integrated Data Repository
The IDR creates an integrated data
environment from Medicare and Medicaid claims, beneficiaries, providers,
Medicare Advantage (MA) plans, Part D Prescription Drug Events (PDEs), and
other data.
The IDR provides greater information
sharing, broader and easier access, enhanced data integration, increased security and privacy, and strengthened query and analytic
capability by building a unified data repository for reporting and analytics.
Now let’s
review the entities that help CMS investigate fraud & abuse activities.
7.15 Investigating Entities

Notes:
Investigating Entities
The following entities review claims
and more extensively investigate specific health care providers:
· UPICs
· Office of
Inspector General (OIG)
· Department
of Justice (DOJ)
· Health Care
Fraud Prevention and Enforcement Action Team (HEAT)
· Federal
Bureau of Investigation (FBI)
These entities work with the claim reviewing
entities and CMS to protect the Medicare Program against fraud & abuse.
Medicare Advantage (MA) plans also
investigate Medicare Part C fraud & abuse. Prescription Drug Plans (PDPs)
investigate Medicare Part D fraud & abuse. Medicare Drug Integrity
Contractors (MEDICs) investigate Medicare Part C and Part D fraud & abuse.
7.16 Unified Program Integrity Contractors

Notes:
Unified Program Integrity
Contractors
UPICs identify suspected fraud &
abuse cases and refer them to the OIG. UPICs may also act to minimize potential
losses to the Medicare Trust Fund and protect Medicare beneficiaries from
potential adverse effects. Appropriate action varies from case to case. For
example, when a provider’s employee files a complaint, the UPIC
immediately advises the OIG.
For more information, go to the Medicare Program Integrity Manual, Chapter 4.
7.17 Office of Inspector General

Notes:
Office of Inspector General
The OIG
protects the integrity of HHS programs, including Medicare, and the health and
welfare of its beneficiaries. The OIG carries out its duties through a
nationwide network of audits, investigations, inspections, and other related
functions. The OIG can exclude individuals and entities who engaged in fraud or
abuse from participation in all Federal health care programs and impose Civil
Monetary Penalties (CMPs) for certain Federal health care program misconduct.
7.18 Department of Justice

Notes:
Department of Justice
The DOJ investigates and prosecutes
fraud & abuse in Federal government programs. The DOJ’s investigators
partner with the OIG; the FBI; and other Federal, State, and local law
enforcement offices through HEAT to investigate and prosecute Medicare fraud
& abuse. DOJ attorneys, through the U.S. Attorney’s Offices, handle
the civil and criminal prosecutions.
7.19 Health Care Fraud Prevention and Enforcement Action Team

Notes:
Health Care Fraud Prevention and
Enforcement Action Team
The DOJ and HHS established HEAT to
build and strengthen existing programs to combat Medicare fraud while investing
new resources and technology to prevent fraud & abuse. HEAT investigators
use new state-of-the-art technology to fight fraud with unprecedented speed and
efficiency.
7.20 Medicare Fraud Strike Force

Notes:
Medicare Fraud Strike Force
The DOJ-HHS Medicare Fraud Strike
Force also fights fraud. Each Medicare Fraud Strike Force team combines the
FBI’s investigative and analytical resources with HHS-OIG’s
Criminal Division’s Fraud Section and the U.S. Attorney’s Offices
prosecutorial resources.
Editable content from image:
Strike Force Statistics
Since Inception
· Cases
Filed: 1,750
· Defendants
Charged: 3,800
· Defendants
Billed Medicare: $15 billion
7.21 Lesson 4: Summary

Notes:
Lesson 4: Summary
· Medicare fraud &
abuse data helps guide claims reviewers and investigators to high-risk fraud
& abuse areas.
· MACs and UPICs
conduct pre-payment claims reviews.
· MACs, the SMRC,
UPICs, CERT Contractors, and RAC Auditors conduct post-payment claims reviews.
· UPICs, OIG, DOJ,
and HEAT investigate Medicare fraud & abuse.
7.22 Lesson 4 Review Title Card

Notes:
Review Questions
Lesson 4: Medicare Anti-Fraud and
Abuse Partnerships and Agencies
After selecting an answer for a
question, select Submit Answer for feedback on the correct answer.
7.23 Review Question 1

Notes:
Review Question 1
Select the correct answer.
You can help prevent Medicare fraud
& abuse by __________.
· A. Medicare
Administrative Contractors (MACs)
· B. Comprehensive
Error Rate Testing (CERT) Contractors
· C. Recovery Audit
Program Recovery Auditors
· D. All of the above
7.24 Review Question 2

Notes:
Review Question 2
Select the correct answer.
Which of the following entities
investigate health care providers suspected of Medicare fraud & abuse?
· A. Office of Inspector
General (OIG)
· B. Department of
Justice (DOJ)
· C. Unified Program
Integrity Contractors (UPICs)
· D. B and C
· E. A, B, and C
7.25 You’ve completed Lesson 4: Medicare Anti-Fraud and Abuse Partnerships and Agencies

Notes:
You’ve completed Lesson
4: Medicare Anti-Fraud and Abuse Partnerships and Agencies
Now that you’ve
learned about the basic concepts of Medicare fraud & abuse detection,
let’s look at how to report Medicare fraud & abuse.
Select the Continue Arrow to return
to the Course Menu. Then, select Lesson 5: Report Suspected Medicare Fraud
& Abuse.
8. Lesson 5
8.1 Lesson 5 Title Card

Notes:
Medicare Fraud & Abuse: Prevent,
Detect, Report
Lesson 5: Report Suspected Medicare
Fraud & Abuse
8.2 Lesson 5 Review

Notes:
Lesson 5: Report Suspected Medicare
Fraud & Abuse
In this lesson, you’ll
learn about reporting fraud & abuse. It should take about 5 minutes to
complete.
In this lesson, you’ll
learn about:
· How you can report
suspected Medicare fraud & abuse
· How you can
self-disclose Medicare fraud & abuse
· The Medicare
Incentive Reward Program (IRP)
8.3 Lesson 5: Learning Objectives

Notes:
Lesson 5: Learning Objectives
After completing this lesson, you
should correctly:
· Recognize how to
report suspected Medicare fraud & abuse
· Recognize how to self-disclose
Medicare fraud & abuse
8.4 How to Report Suspected Medicare Fraud & Abuse: OIG

Notes:
How to Report Suspected Medicare
Fraud & Abuse: OIG
The Office of Inspector General
(OIG) maintains a hotline and webpage that accepts and reviews tips from all
sources, such as Medicare and Medicaid beneficiaries and providers. You can
report suspected fraud & abuse anonymously by phone (OIG Hotline), email,
fax, mail, and on the OIG website. The OIG collects no information that could
trace the complaint to you; however, lack of contact information may prevent a
comprehensive review of the complaint. OIG encourages you to provide contact
information for follow-up.
Use Job Aid E
to report fraud & abuse to the appropriate authorities.
8.5 How to Report Suspected Medicare Fraud & Abuse: MAC

Notes:
How to Report Suspected Medicare
Fraud & Abuse: MAC
For questions about Medicare billing
procedures, billing errors, or questionable billing practices, contact your Medicare Administrative Contractor (MAC).
8.6 What to do if you Suspect you have Problematic Relationships or Inappropriate Billing Practices:

Notes:
What to do if you Suspect you have
Problematic Relationships or Inappropriate Billing Practices:
· Stop submitting
problematic bills
· Seek legal counsel
· Determine money
collected in error from patients and from Federal health care programs and
report and return refunds
· Cease involvement
in a problematic investment
· Get out of the
problematic relationship(s)
· Consider
self-disclosing the issues
8.7 How to Self-Disclose Medicare Fraud & Abuse to the OIG

Notes:
How to Self-Disclose Medicare Fraud
& Abuse to the OIG
Providers who wish to voluntarily
disclose evidence of potential fraud, where it may trigger Civil Monetary
Penalties (CMPs), may do so under the OIG Provider Self-Disclosure Protocol
(SDP). Self-disclosure gives providers the opportunity to minimize the costs
and disruptions associated with a government-directed investigation and civil
or administrative litigation.
The OIG works cooperatively with forthcoming,
thorough, and transparent providers in their disclosures to resolve these
matters. While the OIG does not speak for the Department of Justice (DOJ) or
other agencies, the OIG consults with these agencies, as appropriate, regarding
SDP issues resolution.
Visit the OIG Self-Disclosure Information webpage for more information or to
complete your self-disclosure online.
8.8 How to Self-Disclose Actual or Potential Violations of the
Physician Self-Referral Law (Stark Law)

Notes:
How to Self-Disclose Actual or
Potential Violations of the Physician Self-Referral Law (Stark Law)
For Physician Self-Referral Law
(Stark Law) actual or potential violations, Centers for Medicare & Medicaid
Services (CMS)
Self-Referral Disclosure Protocol (SRDP) allows health
care providers and suppliers to self-disclose them through a separate
OIG process.
The physician cannot use the SRDP to
get a CMS determination as to whether an actual or potential violation of the
Physician Self-Referral Law (Stark Law) occurred. Providers and suppliers
should submit their overpayment liability exposure to the SRDP to resolve the
conduct they identify.
Under certain circumstances, CMS can
reduce the amount due. However, fraud & abuse self-disclosure does not
protect health care providers from sanctions and prosecutions.
8.9 Medicare Incentive Reward Program

Notes:
Medicare Incentive Reward Program
CMS established the Medicare IRP to
encourage reporting suspected fraud & abuse.
The IRP rewards information on
Medicare fraud & abuse or other punishable activities. The information must
lead to a minimum Medicare recovery of $100 from individuals and entities CMS
determines committed fraud.
For more information, go to the Medicare Program Integrity Manual, Chapter 4, Section 4.9.
8.10 Lesson 5: Summary

Notes:
Lesson 5: Summary
· You may report
suspected Medicare fraud & abuse by phone, email, fax, mail, and on the OIG
website.
· You may
self-disclose fraud & abuse to the OIG using the Provider SDP. You may
self-disclose actual or potential violations of the Physician Self-Referral Law
(Stark Law) to CMS using the Medicare SRDP.
· The Medicare IRP
provides rewards for Medicare fraud & abuse information or other punishable
activities.
8.11 Lesson 5 Review Title Card

Notes:
Review Questions
Lesson 5: Report Suspected Medicare
Fraud & Abuse
After selecting an answer for a
question, select Submit Answer for feedback on the correct answer.
8.12 You may report suspected fraud & abuse anonymously by phone, email, fax, mail, and on the Office of Inspector General (OIG) website.

Notes:
Review Question 1
Select the correct answer.
You may report suspected fraud &
abuse anonymously by phone, email, fax, mail, and on the Office of Inspector
General (OIG) website.
· True
· False
8.13 Health care providers who self-disclose fraud & abuse violations are protected from sanctions and prosecutions.

Notes:
Review Question 2
Select the correct answer.
Health care providers who
self-disclose fraud & abuse violations are protected from sanctions and
prosecutions.
· True
· False
8.14 You’ve completed Lesson 5: Report Suspected Medicare Fraud & Abuse.

Notes:
You’ve completed Lesson
5: Report Suspected Medicare Fraud & Abuse.
Now that you’ve
learned about Medicare fraud & abuse prevention, detection, and reporting,
let’s take an assessment to see how much you’ve learned.
Select the Continue Arrow to return
to the Course Menu. Then, select Assessment.
9. Assessment
9.1 Assessment Title Card

Notes:
Assessment
9.2 Lesson 5 Review

Notes:
Assessment
Let’s see how much
you’ve learned. This assessment asks you 10 Medicare Fraud & Abuse:
Prevent, Detect, Report questions. Your estimated completion time is 15
minutes.
You can change your answer until you
select Submit Answer. Once you select Submit Answer, you can’t
change your answer. After selecting Submit Answer and reviewing the answer
feedback, select Next to continue. Once you select Next, you can’t
exit and save your progress.
After successfully completing the
course, you’ll get instructions on how to get a
certificate. Successfully completing the course includes completing all lessons
and a passing assessment grade of at least 70%.
Select Next to begin the assessment.
9.3 Assessment Question 1 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 1 of 10
Select the correct answer.
The Federal laws that address fraud
& abuse include __________.
· A. False Claims Act
(FCA)
· B. Anti-Kickback
Statute
· C. Physician
Self-Referral Law (Stark Law)
· D. Civil Monetary Penalties
Law (CMPL)
· E. All of the above
9.4 Assessment Question 2 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 2 of 10
Select the correct answer.
Health care providers can prevent
fraud & abuse in the Medicare Program by __________.
· A. Not selling free
samples from vendors
· B. Carefully reviewing
business ventures to avoid violating the Anti-Kickback Statute
· C. Reviewing
training and educational materials on Medicare policy on the Medicare Learning
Network® (MLN)
· D. All of the above
9.5 Assessment Question 3 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 3 of 10
Select the correct answer.
You can help prevent Medicare fraud
& abuse by properly and thoroughly documenting all services provided to
Medicare beneficiaries.
· True
· False
9.6 Assessment Question 2 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 4 of 10
Select the correct answer.
A chiropractor, in an intentional
attempt to falsely get Medicare Program money, billed medically unnecessary
services and falsified the beneficiary’s Medicare claim diagnosis.
Depending on the facts and circumstances, she most likely committed __________.
· A. A violation of
the Anti-Kickback Statute
· B. A violation of
the Physician Self-Referral Law (Stark Law)
· C. Medicare fraud
or abuse because she knowingly submitted false Medicare Program claims
9.7 Assessment Question 3 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 5 of 10
Select the correct answer.
Medicare abuse includes any practice
inconsistent with the goals of providing patients with all requested services,
meeting professionally recognized standards, and charging fair prices.
· True
· False
9.8 Assessment Question 6 of 10
(Multiple Choice, 10 points, 1 attempt permitted)

Notes:
Question 6 of 10
Select the correct answer.
You may report suspected fraud &
abuse anonymously to the Office of Inspector General (OIG) via __________.
· A. Phone or fax
· B. Email or mail
· C. OIG website
· D. All of the above
9.9 Assessment Question 6 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 7 of 10
Select the correct answer.
You can help prevent Medicare fraud
& abuse by __________.
· A. Checking the
Office of Inspector General List of Excluded Individuals/Entities (LEIE) before
entering employment or contractual relationships with individuals or entities
· B. Providing
Medicare beneficiaries only medically necessary, high-quality services
· C. Properly
documenting all Medicare beneficiary services provided
· D. All of the above
9.10 Assessment Question 3 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 8 of 10
Select the correct answer.
Health care providers use the
Self-Referral Disclosure Protocol (SRDP) to report all suspected fraud &
abuse.
· True
· False
9.11 Assessment Question 1 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 9 of 10
Select the correct answer.
Possible Medicare fraud & abuse
penalties include __________.
· A. Imprisonment in
criminal cases
· B. Civil Monetary
Penalties (CMPs) up to $100,000 (in 2018) per violation and assessments of up
to 3 times the amount claimed for the item, service, or remuneration offered,
paid, solicited, or received
· C. Exclusion from
participation in all Federal health care programs
· D. A, B, and C
9.12 Assessment Question 10 of 10
(Multiple Choice, 10 points, 1 attempt
permitted)

Notes:
Question 10 of 10
Select the true statement.
· A. Medicare
Administrative Contractors (MACs), Comprehensive Error Rate Testing (CERT)
Contractors, and the Office of Inspector General (OIG) review only claims and
do not investigate health care providers suspected of Medicare fraud &
abuse.
· B. MACs, CERT Contractors,
and the OIG investigate only health care providers suspected of Medicare fraud
& abuse and do not review claims.
· C. MACs, CERT
Contractors, and Recovery Audit Program Recovery Auditors review only claims
and generally do not investigate health care providers suspected of Medicare
fraud & abuse.
· D. MACs, CERT
Contractors, and Recovery Audit Program Recovery Auditors investigate only
health care providers suspected of Medicare fraud & abuse and do not review
claims.