This Initiative was possible through the collaboration of the CMS Innovation Center and the CMS Medicare-Medicaid Coordination Office.
This effort aimed to improve the quality of care for people residing in long-term care (LTC) facilities by reducing avoidable hospitalizations.
CMS supported six organizations that each partnered with a group of LTC facilities to implement evidence-based clinical and educational interventions that both improved care and lowered costs. The Initiative focused on long-stay LTC facility residents who were enrolled in both the Medicare and Medicaid programs, with the goal of reducing potentially avoidable inpatient hospitalizations.
Under this second phase, announced in 2015, the six organizations tested whether a new payment model for LTC facilities and practitioners, together with the clinical and educational interventions in place under the previous phase, could improve quality of care by reducing avoidable hospitalizations while also lowering combined Medicare and Medicaid spending. This phase began in October 2016, at the conclusion of the initial phase, and was expected to last four years.
The Initiative allowed CMS to test the payment model both on its own and in conjunction with the previously-developed clinical and educational interventions.
The intent of the new payment model was to reduce the financial incentive for hospitalization and provide funding for LTC facilities to provide treatment should a beneficiary experience an acute change in condition. LTC facilities were expected to invest the additional resources to implement programs and enhance the skills of staff in order to provide higher intensity services within the facility, thereby reducing avoidable hospitalizations.
New cooperative agreements were announced on March 24, 2016.
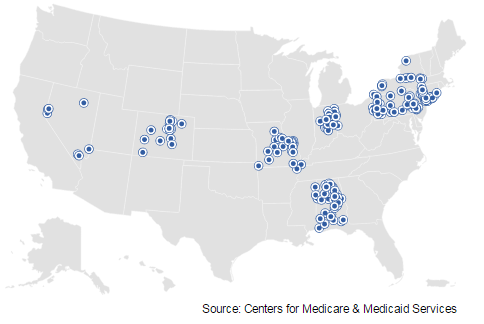
There were 247 long-term care facility participants in the Initiative to Reduce Avoidable Hospitalizations Among Nursing Facility Residents: Phase Two.
Six organizations participating in the Initiative were offered cooperative agreements for the second phase of this Initiative:
Alabama Quality Assurance Foundation – Alabama
HealthInsight of Nevada – Nevada and Colorado
Indiana University – Nevada
The Curators of the University of Missouri – Missouri
The Greater New York Hospital Foundation, Inc. – New York City
UPMC Community Provider Services – Pennsylvania
Background
LTC facility residents often experience potentially avoidable inpatient hospitalizations. These hospitalizations are expensive, disruptive, and disorienting for seniors and people with disabilities. LTC facility residents are especially vulnerable to the risks that accompany hospital stays and transitions between LTC facilities and hospitals, including medication errors and hospital-acquired infections.
Many LTC facility residents are enrolled in both the Medicare and Medicaid programs (Medicare-Medicaid enrollees). Past CMS research on Medicare-Medicaid enrollees in LTC facilities found that approximately 45% of hospital admissions among individuals receiving either Medicare skilled nursing facility services or Medicaid nursing facility services could have been avoided, accounting for 314,000 potentially avoidable hospitalizations and $2.6 billion in Medicare expenditures in 2005.
Research has linked six conditions to approximately 80% of potentially avoidable hospitalizations among LTC facility residents:
| Condition | Percentage |
| Pneumonia | 32.8% |
| Dehydration | 10.3% |
| Congestive Heart Failure (CHF) | 11.6% |
| Urinary Tract Infection (UTI) | 14.2% |
| Skin ulcers, cellulitis | 4.9% |
| COPD, asthma | 6.5% |
| Total | 80.3% |
Initiative Details
From September 2012 to September 2016, under phase one of the Initiative, CMS partnered with seven Enhanced Care and Coordination Provider (ECCP) organizations to improve care for long-stay nursing facility residents.
The intent of the new payment model under the second phase of the Initiative was to reduce potentially avoidable hospitalizations by funding higher-intensity treatment services for residents who may otherwise be hospitalized upon an acute change in condition for any of the six conditions listed above. Improving the capacity of LTC facilities to treat common medical conditions as effectively as possible in-house, as appropriate, has the potential to improve the residents’ care experience at lower cost than a hospital admission. The model also included payments to practitioners (i.e., physicians, nurse practitioners and physician assistants) at levels similar to the payments they would have received for treating beneficiaries in a hospital.
The four-year payment phase of the Initiative was subject to a rigorous external evaluation. Successful ECCP applicants implemented the payment model within partnering facilities from Phase One, where they continued to provide training and clinical interventions, and in a comparable number of newly recruited facilities. ECCPs were responsible for recruiting and screening new providers for participation and ensuring that all providers met readiness standards before receiving any new Medicare funding.
If you have additional questions on this Initiative, please e-mail NFI@cms.hhs.gov. For more information on this initiative, including archived information from both phases, visit the Medicare-Medicaid Coordination Office page.
Evaluations
Latest Evaluation Report
Prior Evaluation Reports
- First Annual Report (PDF)
- Two Pager: Second Annual Findings-At-A-Glance Report (PDF)
- Two Pager: Third Annual Findings At-A-Glance Report (PDF)
- Two Pager: Fourth Annual Findings At-A-Glance Report (PDF)