The mandatory Transforming Episode Accountability Model (TEAM) will advance the Innovation Center’s prior work on episode-based alternative payment models, including the Bundled Payments for Care Improvement Advanced and Comprehensive Care for Joint Replacement Models. The model will launch on January 1, 2026, and run for five years, ending on December 31, 2030. As a mandatory model, all model policies are proposed and finalized through rulemaking. TEAM was designed based on lessons learned from previous episode-based payment models and from input from stakeholders in response to a Request For Information published in 2023.
Model Overview
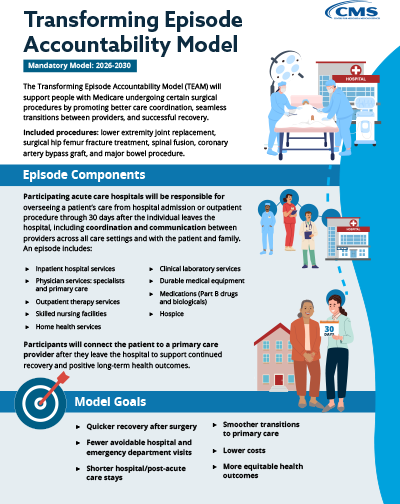
The Transforming Episode Accountability Model (TEAM) will be a mandatory, episode-based, alternative payment model, in which selected acute care hospitals will coordinate care for people with Traditional Medicare undergoing one of the surgical procedures included in the model (initiate an episode) and assume responsibility for the cost and quality of care from surgery through the first 30 days after the Medicare beneficiary leaves the hospital. CMS used Core-Based Statistical Areas (CBSAs) to identify selected geographic regions for the model test. Hospitals paid under the Inpatient Prospective Payment System (IPPS) and located in the selected CBSAs are required to participate in TEAM. The list of selected mandatory CBSAs was published in the final rule. CMS will also allow a one-time voluntary opt-in opportunity for hospitals participating until the last day of the last performance period in the BPCI Advanced model, or the last day of the last performance year in in the CJR model, to participate in TEAM.
As part of taking responsibility for cost and quality during the episode, participants will connect patients to primary care services to help establish accountable care relationships and support optimal, long-term health outcomes. The surgical procedures included in the model will be lower extremity joint replacement, surgical hip femur fracture treatment, spinal fusion, coronary artery bypass graft, and major bowel procedure. For purposes of TEAM, CMS will provide participants with a target price that will represent most Medicare spending during an episode of care, which will include the surgery (including the hospital inpatient stay or outpatient procedure) and items and services following hospital discharge, such as skilled nursing facility stays or provider follow-up visits. Holding participants accountable for all the costs of care for an episode may incentivize care coordination, improve patient care transitions, and decrease the risk of avoidable readmission. In addition, TEAM includes a voluntary Decarbonization and Resilience Initiative, through which CMS will assist participants in increasing quality of care by addressing threats to patient health and the health care system presented by climate change.
Highlights |
|---|
|
Model Purpose
People with Traditional Medicare undergoing a surgical procedure either in the hospital or as an outpatient may experience fragmented care that can lead to complications in recovery, avoidable hospitalization, and other high costs. This is because in a fee-for-service (FFS) payment system, providers and suppliers are paid separately for each service and procedure, potentially resulting in fragmented care, duplicative use of resources, and avoidable utilization. TEAM will test an episode-based payment approach in which acute care hospitals participating in the model, identified as TEAM participants, will receive a target price to cover all costs associated with the episode of care, including the cost of the hospital inpatient stay or outpatient procedure and items and services following hospital discharge, such as skilled nursing facility stays or provider follow-up visits. Through the target price, CMS will hold TEAM participants accountable for spending and quality performance, which can motivate health care providers to better coordinate care and improve the quality of care. TEAM may benefit people with Traditional Medicare who receive one of the included surgical procedures by potentially improving care transitions, encouraging provider investment in health care infrastructure and redesigned care processes, and incentivizing higher value care across the inpatient and post-acute care settings for the episode. Five different surgical procedures will be included in TEAM: lower extremity joint replacement, surgical hip femur fracture treatment, spinal fusion, coronary artery bypass graft, and major bowel procedure.
Model Design
TEAM will be a five-year, mandatory episode-based payment model that will start in January 2026. Hospitals required to participate will be based on selected geographic regions, CBSAs, from across the United States. Additionally, hospitals that participate until the last day of the last performance period of the BPCI Advanced model or the last day of the last performance year of the CJR model will be eligible for a one-time opportunity to voluntarily opt in to TEAM, encouraging these hospitals to maintain their momentum in value-based care. The TEAM design includes a one-year glide path available to all TEAM participants, which will allow TEAM participants to ease into full financial risk. TEAM will have three participation tracks: Track 1 will have no downside risk and lower levels of reward for the first year, or up to three years for safety net hospitals; Track 2 will be associated with lower levels of risk and reward for certain TEAM participants, such as safety net hospitals or rural hospitals, for years 2 through 5; and Track 3 will be associated with higher levels of risk and reward for years 1 through 5.
Episodes will begin with a hospital inpatient stay or a hospital outpatient procedure for one of the following surgical procedures: lower extremity joint replacement, surgical hip femur fracture treatment, spinal fusion, coronary artery bypass graft, and major bowel procedure. Each episode would end 30 days after the individual leaves the hospital.
TEAM participants will continue to bill Medicare FFS as usual but will receive target prices for included episodes prior to each performance year. Target prices will be based on all Medicare Parts A & B items and services included in an episode and will be risk-adjusted based on beneficiary-level and hospital-level factors. Performance in the model will be assessed by comparing the participants’ actual Medicare FFS spending for the episode to their target price, as well as through an assessment of performance on specific quality measures. TEAM participants may earn a payment from CMS, subject to a quality performance adjustment, if the total Medicare costs for the episode are below the target price. TEAM participants may owe CMS a repayment amount, subject to a quality performance adjustment, if the total Medicare costs for the episode are above the target price.
Notably, and consistent with the CMS Innovation Center strategy to drive accountable care and integrate specialty care and primary care, the model is designed to complement longitudinal care management through policies that align with Accountable Care Organizations (ACOs) and promote primary care referral. Under TEAM, a person receiving care from (aligned to) providers in an ACO will be in an episode if they receive one of the surgeries included in TEAM at a hospital that is participating in TEAM. Allowing a person with traditional Medicare to be included in both TEAM and ACO initiatives will help to promote provider collaboration to find opportunities to improve quality of care and reduce Medicare spending. Also, TEAM will require hospitals to refer patients to primary care services to support continuity of care and positive long-term health outcomes.
Health Equity Strategy
TEAM will support CMS’ broader efforts to promote health equity to ensure all populations can achieve optimal health through increasing access to quality care. The model will offer certain flexibilities to help participants that care for a higher proportion of underserved individuals, such as safety net hospitals, by reducing the financial burden sometimes associated with value-based model participation. This includes the option to participate in Tracks 1 and 2 of TEAM, which have lower financial risks and rewards as compared to Track 3, in that the amount of money the TEAM participant may be required to repay CMS or earn from CMS is limited. The model’s target pricing methodology will also include a social risk adjustment to ensure target prices properly reflect the additional financial investment needed to care for underserved individuals. To address disparities and support continuous quality improvement, participants may voluntarily submit health equity plans to CMS and report demographic data to CMS. TEAM participants may also voluntarily screen and report individuals for health-related social needs.
Decarbonization and Resilience Initiative
TEAM will also support CMS and HHS efforts to improve quality of care by bolstering the health system’s climate resilience and sustainability by assisting TEAM participants in addressing threats to patient health and the health care system presented by climate change. CMS will allow TEAM participants to voluntarily report metrics related to greenhouse gas emissions to CMS, and CMS will provide individualized feedback reports to TEAM participants as well as public recognition of their participation in the initiative. Further, TEAM participants will have access to technical assistance and learning resources to help enhance organizational sustainability, support care delivery methods that may lower greenhouse gas emissions, and identify tools to measure emissions.
Additional Information
- TEAM Participant List (XLSX) - updated September 2024
- 2025 IPPS Final Rule
- TEAM Fact Sheet (PDF)
- TEAM Decarbonization and Resilience Initiative
- TEAM Press Release
- TEAM Frequently Asked Questions
- TEAM infographic (PDF)
- IPPS Proposed Rule
- The CMS Innovation Center’s Strategy To Support Person-Centered, Value-Based Specialty Care: 2024 Update
Outreach
If you are interested in receiving additional information, updates or have questions about the Transforming Episode Accountability Model (TEAM), please see the resources below:
- Email: CMMI_TEAM@cms.hhs.gov
- Sign up for updates from the Transforming Episode Accountability Model (TEAM)
- TEAM Primary Point of Contact Identification Form - representative from each hospital selected for mandatory TEAM participation should complete this form to identify points of contact for TEAM-related communications