Published August 14, 2023
Defining key terms: |
|---|
|
What’s the relationship between health equity and health disparities?
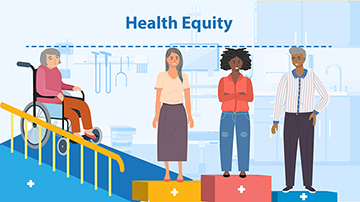
Health equity is when everyone has a fair and just opportunity to attain their optimal health.
Health equity is advanced when care providers:
- Identify health disparities
- Define specific and actionable goals for addressing any disparities identified
- Prioritize populations and communities that are historically underserved
- Establish and implement their organization’s health equity strategy
- Determine what tools and resources their organization needs to implement its strategy
- Monitor and evaluate progress in addressing health disparities
Health disparities occur when an underserved group with a shared characteristic – such as race or disability – is impacted by a preventable health issue more frequently or more severely than individuals that do not share in that characteristic. Often, these populations have been historically excluded from social and economic opportunities, resulting in barriers to care and unequal treatment over time. We’re committed to addressing the health disparities that underlie our health system.
Recognizing and addressing the issues that contribute to health disparities will help achieve health equity
Examples of efforts to advance health equity
Partners in preventive care
A rural community relies heavily on their local volunteer fire department (VFD) during health emergencies because the nearest hospital is more than 20 miles away. However, the VFD doesn’t have the same services or specialized-trained staff as a health clinic. Additionally, many health emergencies in this community could be avoided if they had access to preventive services, like health screenings, smoking cessation programs and nutrition support.
To help address these health disparities and advance health equity, a health clinic from a relatively nearby city partners with and provides the VFD with health care training, equipment, and services. In addition, clinicians come to the VFD the first and third Thursday of every month to supply the community with convenient and high-quality preventive care, like blood pressure screenings and mental health evaluations. The health clinic also offers telehealth visits to reduce transportation burdens.
Community collaboration
A health system meets with church and other community leaders who primarily serve a large urban African American community with a high prevalence of chronic heart disease to determine how they can help address this health disparity. Working closely with church leaders to understand the community’s needs and priorities, the health system enters into a jointly-designed learning collaborative. The collaborative engages churches across the area, each of which sets its own goals to encourage its members to adopt healthy lifestyle changes to improve heart health. The health system, in turn, supports these churches by holding health education sessions and conducting health screenings. To help monitor impact, the churches provide progress reports on key metrics that determine whether these efforts affect changes in health outcomes.
Our Commitment to Advancing Health Equity
Here are some ways we’re advancing health equity:
- Designing, implementing, and operationalizing policies and programs that support health for all the people served by our programs
- Eliminating avoidable differences in health outcomes experienced by people who are disadvantaged or underserved.
- Providing the care and support that our enrollees need to thrive.
- Supporting providers who work in underserved communities – known as safety net providers – and encouraging them to participate in CMS Innovation Center models that test ways we can improve the quality of care for all patients.
- Including diverse patient perspectives in every phase of a CMS Innovation Center model – from development, to implementation, to evaluation – to ensure models best serve all patients’ needs.
CMS Innovation Center models and initiatives that focus on advancing health equity
Learn more about CMS Innovation Center models and initiatives that aim to improve health equity. These models provide underserved communities with services to help increase the quality of their care:
- Community Health Access and Rural Transformation (CHART) Model
- End-Stage Renal Disease Treatment Choices (ETC) Model
- Pennsylvania Rural Health Model
- Maternal Opioid Misuse (MOM) Model
- Integrated Care for Kids (InCK) Model
- Accountable Health Communities (AHC) Model
- Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model
- Maryland Total Cost of Care (TCOC) Model
For more information about the CMS Innovation Center’s new strategy and the future of value-based care, visit our Strategic Direction webpage.
You can also learn about the CMS Office of Minority Health’s Health Equity Programs.