Accountable Care Organization (ACO) Human-Centered Design Customer Engagement
Accountable Care Organization (ACO) Human-Centered Design Customer Engagement
Human-Centered Design (HCD) is the process CMS uses to understand the people for which we are writing policies and creating programs and services. At the center of CMS’ HCD process is participatory design, where we work directly with clinicians, patients, third-party vendors, federal partners, and CMS employees to collaboratively understand the context of their work and engagement with CMS, as well as the solutions we are creating to support them.
Engaging partners and the communities CMS serves is a core part of the agency's strategic plan. As part of this work, we aim to keep channels of communication open to ensure your voices are heard and considered in everything we do, particularly as we design and implement new programs and initiatives.
In early 2022, the CMS conducted an Accountable Care Organization (ACO) Human-Centered Design Customer Engagement focused on identifying the human experience of ACO participants and other stakeholders by understanding barriers when reporting aggregate electronic Clinical Quality Measures (eCQMs) and Merit-based Incentive Payment System (MIPS) CQMs. Our research included extensive interviews with a broad range of stakeholders, including ACOs, health IT vendors, and advocacy organizations.
ACOs are groups of doctors, hospitals, and other health care providers who come together voluntarily to give coordinated high-quality care to the Medicare patients they serve. Coordinated care helps ensure that patients, especially the chronically ill, get the right care at the right time, with the goal of avoiding unnecessary duplication of services and preventing medical errors.
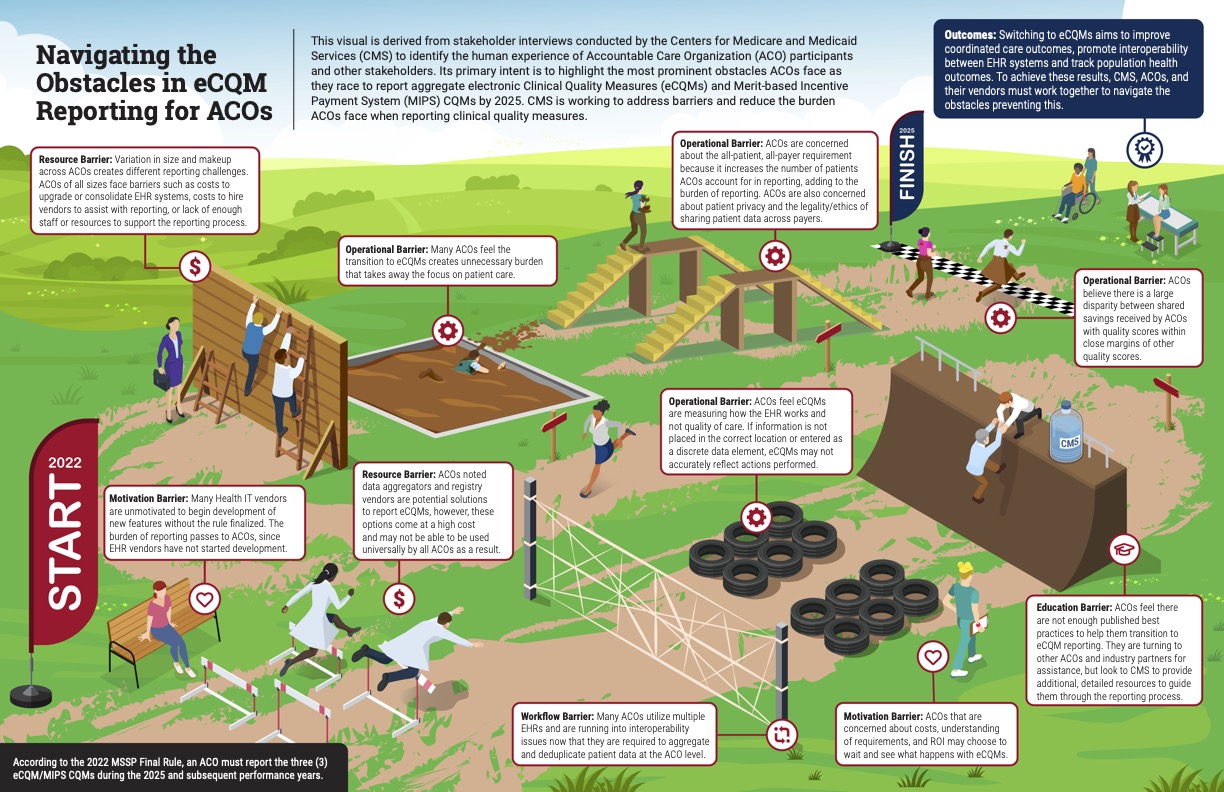
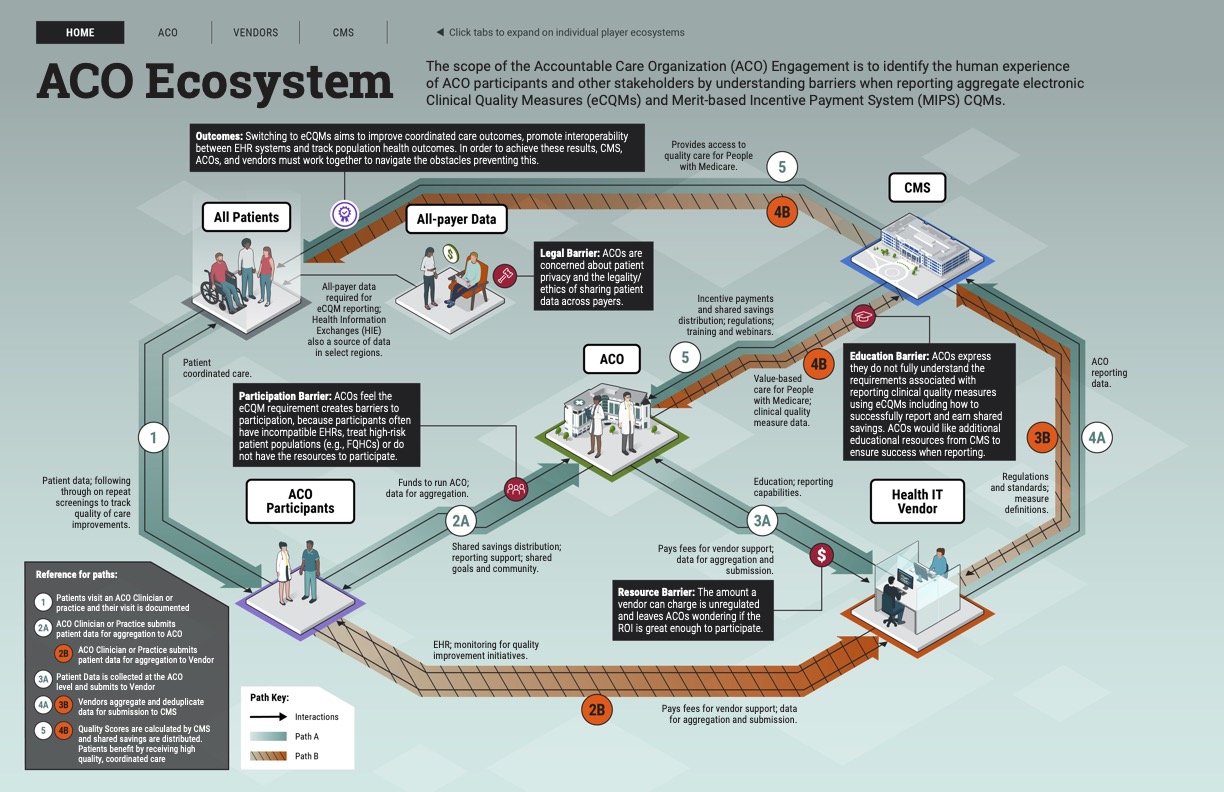
Two illustrations were also co-created to represent insights from our customers: “Navigating the Obstacles in eCQM Reporting for ACOs” and the “ACO Ecosystem.”
The primary intent of “Navigating the Obstacles in eCQM Reporting for ACOs” is to highlight the most prominent difficulties ACOs face as they race to report aggregate electronic Clinical Quality Measures (eCQMs) and Merit-based Incentive Payment System (MIPS) CQMs by 2025.
The “ACO Ecosystem” illustrates the relationships and interactions between ACOs, ACO participants, patients, Health IT vendors, and CMS, including challenges encountered as part of the eCQM reporting process.
The ACO Customer Engagement supports and informs the development and direction of the CMS Quality Payment Program (QPP) Strategy. CMS is working to address barriers and reduce the burden ACOs face when reporting Clinical Quality Measures.