About the CMS Innovation Center
The Center for Medicare and Medicaid Innovation, also known as the CMS Innovation Center, develops and tests new healthcare payment and service delivery models to:
- Improve patient care.
- Lower costs.
- Better align payment systems to promote patient-centered practices.
The CMS Innovation Center’s models are alternative payment models (APMs) which reward health care providers for delivering high-quality and cost-efficient care. APMs can apply to a specific:
- Health condition, like end-stage renal disease.
- Care episode, like joint replacement.
- Provider type, like primary care providers.
- Community, like rural areas.
- Innovation within Medicare Advantage or Medicare Part D.
Watch our video explaining how models test new ways to provide better, more affordable care:
History of the CMS Innovation Center
The CMS Innovation Center was established by Congress in 2010 to identify ways to improve healthcare quality and reduce costs in the Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) programs. Following this charge, the CMS Innovation Center, through its models, initiatives and Congressionally-mandated demonstrations, has accelerated the shift from a health care system that pays for volume to one that pays for value.
Testing New Payment and Service Delivery Models
The CMS Innovation Center leverages expertise from across the health care industry, including clinicians, analysts and beneficiary groups, and other federal agencies in the development of new payment and service delivery models. The CMS Innovation Center welcomes input on model ideas and innovations related to health care service delivery and payment but does not, however, fund unsolicited proposals or provide grants for model development.
The CMS Innovation Center solicits and selects model participants through open competition. The CMS Innovation Center follows protocols to ensure fairness and transparency, and provides potential partners opportunities to ask questions regarding expectations.
Evaluating Results and Advancing Best Practices
The CMS Innovation Center continually monitors and evaluates its payment and service delivery models.
Statute specifies the CMS Innovation Center evaluate quality of care (including patient-level outcomes, patient satisfaction and other patient-centeredness criteria) and changes in spending in each model. The CMS Innovation Center also gathers and reports on lessons-learned and best practices identified during model testing to support improvements across CMS and the health care system, at large. The CMS Innovation Center facilitates and accelerates the healthcare system’s move to value-based care, which pays for healthcare based on outcomes.
The CMS Innovation Center has created learning collaboratives for model participants to promote broad and rapid dissemination of evidence and best practices that have the potential to deliver higher quality and lower cost care for Medicare, Medicaid and CHIP beneficiaries. This includes leveraging claims data and other metrics to deliver actionable feedback to providers about their performance.
Expanding Models
Congress provided the Secretary of Health & Human Services (HHS) the authority to expand the scope and duration of a model through rulemaking, including the option to test a model nationwide. To exercise this authority, the Secretary and CMS actuaries must review the CMS evaluations and determine that a model must either reduce spending without reducing the quality of care, or improve the quality of care without increasing spending, and must not deny or limit the coverage or provision of any benefits.
Quality Payment Program
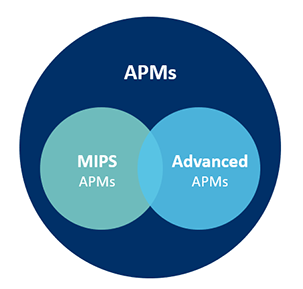
The CMS Innovation Center plays a critical role in implementing the Quality Payment Program, which Congress created as part of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) to replace Medicare’s Sustainable Growth Rate formula to pay for physician and other provider services. In this program, clinicians may earn incentive payments by sufficiently participating in Advanced APMs. By participating in Advanced APMs, clinicians also accept some risk based on their patients’ quality and cost outcomes and other specified criteria.
For more Quality Payment Program resources, please review the QPP Resource Library.
Where Can I Learn More About the CMS Innovation Center?
- CMMI Strategic Direction
- List of innovation models
- Completed Models Contribute to Health System Transformation
- CMS Innovation Center Key Concepts
- Model data and reports
- Recent milestones and updates
- Connect with the CMS Innovation Center
- Learn more about models in your state Please contact your health care provider directly if you have questions about their participation in a CMS Innovation Center model.
Our Team
The Innovation Center is a component of the Centers of Medicare & Medicaid Services, an Agency of the U.S. Department of Health & Human Services. See our general organization structure and read the bios of our leadership. The Innovation Center is directed by Liz Fowler. Learn More about Our Team
Contact CMS
If you have a question about a particular Innovation Model, please find the direct email address for that Model mentioned on its details page. For other inquiries, you can find information about getting in touch with CMS on cms.gov. Learn More
Originally posted on: August 14, 2023 | Reviewed and revised on: August 9, 2024