The Center for Medicare & Medicaid Innovation (CMS Innovation Center) develops payment and delivery models designed to improve the effectiveness and efficiency of specialty care. Among those specialty models was the Oncology Care Model, which aimed to provide higher quality, more highly coordinated oncology care at the same or lower cost to Medicare. Under the Oncology Care Model (OCM), physician practices entered into payment arrangements that included financial and performance accountability for episodes of care surrounding chemotherapy administration to cancer patients. The Centers for Medicare and Medicaid Services (CMS) also partnered with commercial payers in the model. The practices which participated in OCM committed to providing enhanced services to Medicare beneficiaries such as care coordination, navigation, and national treatment guidelines for care.
If you are looking for beneficiary-focused information about OCM, please visit the OCM beneficiary-focused resource on Medicare.gov.
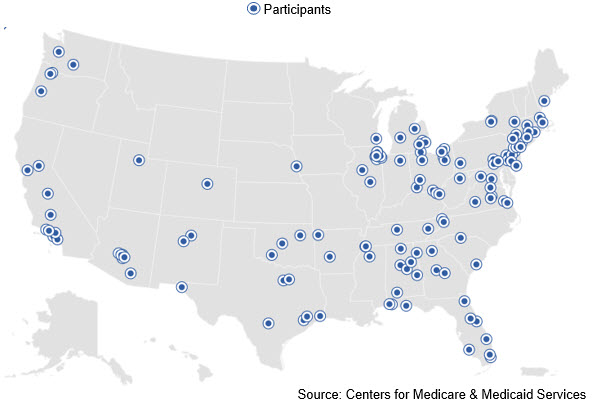
As of June 30, 2022, when the model concluded, there were 122 practices and 5 commercial payers participating in the Oncology Care Model.
The 5 participating payers were:
- Aetna
- BlueCross BlueShield of South Carolina
- Cigna Life & Health Insurance Company
- Priority Health
- The University of Arizona Health Plan
Background
Cancer diagnoses comprise some of the most common and devastating diseases in the United States: more than 1.6 million people are diagnosed with cancer each year in this country. Through OCM, the CMS Innovation Center had the opportunity to achieve three goals in the care of this medically complex population: better care, smarter spending, and healthier people.
Model Details
The goal of OCM was to utilize appropriately aligned financial incentives to enable improved care coordination, appropriateness of care, and access to care for beneficiaries undergoing chemotherapy. OCM encouraged participating practices to improve care and lower costs through an episode-based payment model that financially incentivized high-quality, coordinated care. The CMS Innovation Center expected that these improvements would result in better care, smarter spending, and healthier people. Practitioners in OCM were expected to rely on the most current medical evidence and shared decision-making with beneficiaries to inform their recommendation about whether a beneficiary should receive chemotherapy treatment. OCM provided an incentive to participating physician practices to comprehensively and appropriately address the complex care needs of the beneficiary population receiving chemotherapy treatment, and heighten the focus on furnishing services that specifically improve the patient experience or health outcomes.
Commercial payers participated in OCM in alignment with Medicare to create broader incentives for care transformation at the physician practice level. Aligned financial incentives that resulted from engaging multiple payers leveraged the opportunity to transform care for oncology patients across a broader population. Other payers benefited from savings, better outcomes for their beneficiaries, and greater information around care quality. Participating payers had the flexibility to design their own payment incentives to support their beneficiaries, while aligning with the Innovation Center’s goals for care improvement and efficiency.
OCM incorporated a two-part payment system for participating practices, creating incentives to improve the quality of care and furnish enhanced services for beneficiaries who undergo chemotherapy treatment for a cancer diagnosis. The two forms of payment included a per-beneficiary Monthly Enhanced Oncology Services (MEOS) payment for the duration of the episode and the potential for a performance-based payment for episodes of chemotherapy care. The $160 MEOS payment assisted participating practices in effectively managing and coordinating care for oncology patients during episodes of care, while the potential for performance-based payment incentivized practices to lower the total cost of care and improve care for beneficiaries during treatment episodes.
Evaluations
Latest Evaluation Report
Prior Evaluation Reports
- Two Pager: At-A-Glance Report (PDF)
- Transformation Spotlight: Care Transformation Insights from the Oncology Care Model (PDF)
- Two Pager: At-A-Glance Report (PDF)
- Oncology Care Model - Participant Perspectives Evaluation Report: Periods 1-6 (PDF)
- Two Pager: At-A-Glance Report (PDF)
- Two Pager: At-A-Glance Report (PDF)
- Two Pager: At-A-Glance Report (PDF)
- White Paper - Episode Payment Models Evaluation Synthesis (PDF)
- Second Annual Report Two Pager: At-A-Glance Report (PDF)
- First Annual Report
Additional Information
- Oncology Care Model Fact Sheet
- Oncology Care Model Press Release (06/29/2016)
- Oncology Care Model Press Release (02/12/2015)
- Video: Oncology Care Model Experiences - Northwest Medical Specialties
- Video: Oncology Care Model Experiences - The Center for Cancer and Blood Disorders
- Oncology Care Model beneficiary-focused resource on Medicare.gov
Model Materials
- Oncology Care Model Overview Slides (PDF)
- Oncology Care Model General Program Documents (ZIP)
- Oncology Care Model Data Registry (ZIP)
- Oncology Care Model Key Drivers and Change Package (PDF)
- Oncology Care Model Beneficiary Notification Letter Template (PDF)
- Oncology Care Model Beneficiary Notification Letter Template - Spanish (PDF)
Methodology
- Oncology Care Model Performance Periods 1 and 2 Payment Methodology (PDF)
- Oncology Care Model Performance Period 3 and Forward Payment Methodology (PDF)
- Oncology Care Model Novel Therapy Drug List Effective July 2022 (XLSX)
- Oncology Care Models Initiating Therapies List Effective July 2021 (XLSX)
Data Reporting
Staging and Clinical Data
- Oncology Care Model Staging and Clinical Data (ZIP)
- Oncology Care Model Performance Period 4 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 5 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 6 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 7 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 8 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 9 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 10 Staging and Clinical Data Reporting (ZIP)
- Oncology Care Model Performance Period 11 Staging and Clinical Data Reporting (ZIP)
Quality Measures
- Oncology Care Model Quality Measures (ZIP)
- Oncology Care Model January - June 2019 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model July - December 2019 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model January - June 2020 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model July - December 2020 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model January – June 2021 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model July – December 2021 Measurement Period Aggregate Measure Result Reporting (ZIP)
- Oncology Care Model January – June 2022 Measurement Period Aggregate Measure Result Reporting (ZIP)